Acute prostatitis is an acute inflammation of the prostate caused by infection.With this disease, the prostate swells and foci of pus appear in its tissue.Statistics allow us to assert that acute prostatitis in men is a common disease; the risk of its occurrence increases with age.
The effect of acute prostatitis treatment directly depends on the timeliness of patient treatment.The disease can quickly become chronic, with treatment longer and more complex.
forms of acute prostatitis
If we talk about the clinical development of acute prostatitis in men, the disease is divided into three forms (stages):
- catarrhal disease;
- follicle;
- Parenchyma.
Catarrhal inflammation occurs first and is characterized by acinar dilatation and reactive edema of the interstitial tissue.This causes the prostate to enlarge significantly.The next stage is the rapid spread of the inflammatory process to the prostatic lobules and excretory ducts.We're specifically talking about the prostate's excretory duct that leads to the back of the urethra.Inflammatory changes affect only the mucosa.The excretory ducts lose their contractility, become significantly narrowed, or become completely blocked, thereby impeding the release of prostate secretions.The catarrhal form is directly related to the movement of infectious agents from the posterior urethra.Since the inflammatory process also affects prostatic secretion, posterior urethritis may occur.
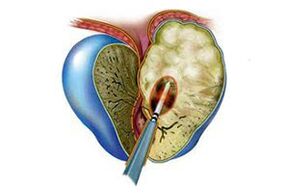
In the follicular stage, inflammatory lesions reach and spread to individual lobules or throughout the prostate.Foci of purulence appear and pus enters the urethra.The enlargement of the prostate does not stop; destructive changes occur in the tissue.
In the parenchymal stage of acute prostatitis, the inflammatory process affects the prostatic stromal tissue.This stage occurs after penetration of infectious agents through contact or the hematogenous route, such as after surgery.
Parenchymal prostatitis is accompanied by the appearance of a single pustule at onset, which in the course of development unites and coalesces with a prostatic abscess.
As for follicular and parenchymal morphology, inflammatory changes often occur in the posterior urethra and bladder neck during development.
Prediction and prevention of acute prostatitis
In the vast majority of cases, timely allotropic treatment can eradicate the signs of acute prostatitis.If left untreated, abscesses are likely to develop or the disease may become chronic.
Preventing this disease usually means prompt treatment of any infectious diseases in the body, as well as the identification and treatment of sexually transmitted diseases and urethritis.Men need to maintain a healthy lifestyle, especially increasing physical activity.Additionally, having regular sex and avoiding unprotected casual contact can prevent the development of this disease.Strict adherence to personal hygiene rules is another important requirement for men of any age.
disease cause
Acute prostatitis in men can occur at any age.The reason is often the invasion of various infectious pathogens.This is E. coli, but it could also be Streptococcus, Staphylococcus, Candida, Chlamydia, Trichomonas.The most common route of entry is through the excretory duct.Pathogens can also enter the prostate from the bladder that is undergoing an inflammatory process (eg, acute cystitis).Infection can also spread from nearby purulent lesions.
The inflammatory process of the prostate caused by the presence of microorganisms can occur for a variety of reasons.Factors that increase risk include:
- Surgical intervention in the urethral region;
- Unprotected sexual intercourse, inflammatory diseases of the partner's genitourinary tract;
- use of urinary catheter;
- Prostate stones, etc.
Acute prostatitis may occur independently of infection.It can occur due to a sedentary lifestyle, hypothermia, and various diseases that cause stagnation in the pelvic area.
Symptoms of acute prostatitis
Since acute prostatitis has different stages, the symptoms of the disease often depend on them.But all forms share some common characteristics.First there is the problem of pain, systemic intoxication and the process of urination.
Catarrhal type is usually accompanied by severe pain, heaviness in the perineum, and frequent and painful urination.During palpation, the doctor may notice an increase in the size of the prostate gland.The results of a secretion test may show high levels of white blood cells.

The symptoms of follicular acute prostatitis are more obvious.Men may experience perineal pain that radiates to the sacrum or penis.The urination process is accompanied by pain, urine retention, and often difficulty in defecation.The patient felt generally unwell and had a fever.Palpation reveals enlargement of the prostate and its outline becomes asymmetrical.Localized pain may occur.Tests showed increased white blood cell levels and strands of pus in the urine.
The substantial form is accompanied by a sharp increase in body temperature, which can reach 39.5 degrees.General symptoms are obvious: chills, loss of appetite and weakness.Urination is delayed and the process is accompanied by severe pain.Defecation is also difficult and constipation becomes severe.
In this case, it is necessary to urgently start treatment for acute prostatitis.If this process begins, there is a high likelihood of prostate abscess, paraprostatitis, paraprostatic plexophlebitis.If patients don't see a doctor, the disease becomes chronic and the likelihood of full recovery is greatly reduced.
Diagnosis of acute prostatitis
When a patient contacts a urologist, the doctor diagnoses acute prostatitis and determines the stage of the disease.Experts receive information after conducting comprehensive research.Diagnosis in this case included physical, instrumental, and laboratory studies.
The physical exam includes studying the condition of the prostate from the rectum.Therefore, the specialist has the opportunity to evaluate the size, shape, consistency of the organ and the presence of pain.As a result of the analysis of the secretions, a decrease in the number of lecithin granules and an increase in the level of white blood cells are easily determined.
Gland palpation also involves collecting and transferring urine for examination.In most cases, acute prostatitis is signaled by elevated levels of white blood cells.Urine culture, PCR and blood culture as well as analysis of urethral secretions are also prescribed.
In the case of this disease, the instrumental approach is represented by transrectal ultrasound diagnosis.If the patient is in severe pain, the transabdominal method is chosen for examination.
When the question of surgical intervention arises, CT and MRI of the pelvis are necessary.
Treatment of acute prostatitis
The treatment of acute prostatitis is carried out in the hospital.This is due to two factors.First, there is a risk of serious complications that may affect men's health, thereby affecting reproductive function and erection quality.Secondly, the condition is complex, the symptoms are obvious, and the pain is strong.The treatment of acute prostatitis starts with drug treatment, prescribing symptomatic drugs to the patient.The most important function is to inhibit the function of microorganisms as antibacterial agents.
To reduce the severity of pain and eliminate spasms, patients are advised to take antispasmodics and analgesics.Hot enemas and rectal suppositories are sometimes used to provide relief.After acute symptoms are overcome, physical therapy may be used.These procedures can increase microcirculation, improve local immunity, and help eliminate inflammation.Among the physical therapy methods for treating acute prostatitis, the most effective are prostate massage, microwave therapy and electrophoresis therapy.Prostate massage has been considered a particularly popular practice for many years to help relieve congestion; it is also recommended for men over forty to use it regularly as a preventative measure.
If there are problems with the urinary process, a urinary catheter is not used; instead, a trocar cystostomy is preferred.
Recovery is considered the regeneration of the prostate tissue, the complete restoration of its functions, while laboratory tests indicate the absence of infectious pathogens and the return of prostate secretions to their normal composition.
Surgery is not a widely used treatment for prostatitis.It doesn't always bring results.Surgical solution resulted in positive dynamics in less than half of the cases.The most common side effect of surgery is erectile dysfunction, and retrograde ejaculation, in which sperm enters the bladder during ejaculation, is also common, and ureteral stricture sometimes occurs.Surgical methods do not guarantee freedom from recurrence.Therefore, surgical intervention is only performed in certain cases, such as:
- When a prostate abscess occurs, it must be opened and cleaned;
- Treatment using conservative methods such as medications, traditional medicine, and physical therapy procedures lacks effectiveness;
- Serious complications occur;
- There are foci of inflammation in the pelvic area;
- Formation of paraproctitis (purulent abscess in the cells surrounding the rectum);
- Presence of blood in urine;
- Delayed urination and cessation of urination (anuria);
- The cause of the presence of stones in the bladder and kidneys is prostatitis;
- Malignancy is suspected.































